- All upper GI endoscopy should be considered high risk and enhanced PPE is recommended for all patients, regardless of any risk stratification.
- BSG also considers lower GI endoscopies to be aerosol generating procedures (AGP) but the evidence for this is less strong and there is insufficient evidence to consider these as high risk at the present time
- Risk stratification of patients by symptoms and temperature is of limited value, given the widespread prevalence and incubation period of up to 14 days
- We recognise the limited availability of PPE, especially FFP3 masks, and so case selection is critical, focussing only on emergency and absolutely essential procedures. Minimising the volume of emergency activity will help preserve PPE supply.
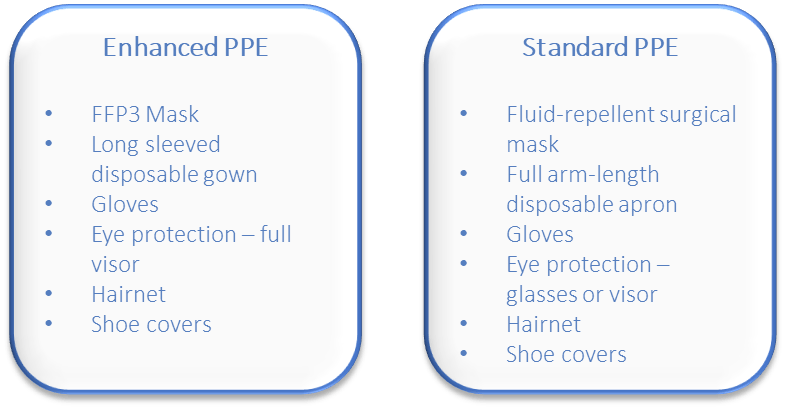
Notes on FFP3 masks and enhanced PPE
- Proper fitting and testing prior to use
- Although ‘single use’ can use for several hours if not removed/contaminated
- FFP3 uncomfortable after prolonged wearing, may affect ease of procedure
- Cannot e.g. use phone, visit, toilet, eat or drink once enhanced PPE is on
- Meticulous removal of enhanced PPE is vital; follow PHE advice
- For COVID-positive patients – consider wearing full visor and surgical mask over FFP3 mask. This minimises risk of contamination of FFP3 mask and prolongs use
Further Key points for Optimal Practice
For known COVID-positive patients
- Scope in designated, different area of the department
- Designated, separate recovery area
- Minimal furniture and equipment in room
- Minimum essential staff in room
Remember
- PPE is only part of the strategy to prevent and control transmission of infection
- Team organisation –essential staff only in procedure room
- Don’t share PCs, keyboards, phones etc – or clean thoroughly between users
The situation is rapidly evolving and this guidance may be updated regularly
